Methods: Between September 2015 and November 2016, a total of 11 patients (8 males, 3 females; mean age: 45.4±12.0 years; range, 23 to 59 years) who underwent lung transplantation with different primary indications were included. The copy numbers of KREC gene segment were quantified using real-time polymerase chain reaction method in peripheral blood samples collected pre- and post-transplantation. The samples of the patients were compared with the KREC l evels i n deoxyribonucleic acid extracted from blood samples of healthy children.
Results: There was no significant change in KREC levels between pre- and post-operation (p=0.594 and p=0.657), although the median values indicated that the highest increase in the KREC levels (7¥105- 12¥105; 85-170) was on Day 7 of transplantation. There was a positive correlation between the KREC levels (mL in blood) and lymphocytes at 24 h after transplantation (p=0.043) and between KREC copies per 106 of blood and age on Day 7.
Conclusion: Our preliminary results suggest that KREC l evels a s an indicator of B lymphocyte production are elevated after lung transplantation. A prognostic algorithm by tracking B cell kinetics after post-transplantation for long-term follow-up can be developed following the confirmation of these preliminary results with more patient samples.
The lung is the one of the largest transplantable organs with an extensive vasculature that is exposed to the entire cardiac output. The lung has also a vast intrinsic immune apparatus, which includes large populations of both antigen-presenting cells and effector cells, and the respiratory tract is in constant contact with extrinsic inhaled antigens, leading to local inflammatory reactions with upregulation of alloantigen expression on bronchial epithelium and activation of T lymphocytes.[3]
Production of B lymphocytes in solid organ transplants to follow the response of the recipient"s immune system can be monitored by measuring kappa-deleting recombination excision circles (KRECs) as in hematopoietic stem cell transplants.[4,5] The KREC is an extrachromosomal circular product. It separates from deoxyribonucleic acid (DNA) due to light chain gene rearrangement in B lymphocyte development, and it is diluted each time the cell is divided.[4] During the maturation processes of B-cell receptor (BcR) heavy and light chains, antigen receptor genomic rearrangements generate functional receptors. This process is necessary, as the gene complexes encoding the BcR components do not contain a functional first exon, while including multiple variable (V), diversity (D), and joining (J) genes. In the antigen-independent differentiation phase, stepwise rearrangements are introduced into the genome to couple one of each segment together to form a functional first exon. B-cell maturation and KRECs are the products of recombination events determining the allelic and isotypic exclusion of the immunoglobulin (Ig) kappa (IGK) locus.[6] Although Igs have two types of light chain, kappa ( κ) and lambda (λ), B lymphocytes express only one of these two types of chains. About 60% of the B lymphocytes in human express χ chain, while 40% have λ chain.[7] When this gene rearrangement is successfully completed in the cell, the B cell enters the germinal center and undergoes somatic hypermutation, resulting in memory or plasma cells with an Igχ light chain.[5,8]
In the present study, we used real-time polymerase chain reaction (PCR) assay to quantify B lymphocyte mobilization through detection of KRECs. The primer and probe final concentrations were described previously by Sottini et al.[9] Standardization of the test procedure was achieved by carrying out specific optimization procedures. We aimed to investigate the possibility of using the KREC levels, as an indicator of B cell kinetics, in follow-up of patients with LTx. We, therefore, report preliminary results from 11 patients in the short term and discuss potential studies in the future.
Preparation of KREC signal joints and reference
gene (T cell receptor alpha constant- TCRAC)
Lymphocyte subpopulations and the population of
naïve B cells defined by CD19 phenotype gradually
decreases with age/age-related accumulation of
immune experience resulting from contact with
foreign antigens. B cells are manifested by a gradual
shift from immature to mature status, with the total
number of B lymphocytes gradually decreasing since
the neonatal period along with an increasing ability to
respond to foreign antigen.[10]
In almost all studies where KREC level is measured, TCRAC is used as the reference gene in the quantitative PCR method.[11-15] T cell receptors (TCR) are very important in Ig synthesis and major histocompatibility complex (MHC)-dependent antigen recognition via B cell. Each TCR gene locus contains V and J gene segments. In addition, as in the Ig gene locus, D segment is present in β and δ regions. The receptor formation of the T cell occurs similar to the V (D) J gene rearrangement in the Ig genes.[7] While the gene segment (TREC) carrying the signal segment in the T cell division does not duplicate itself, the coding segment (TCRAC) is transferred to newly formed cells. The gene rearrangement mechanism in T cells is similar to formation of immunoglobulins. Since TCRAC has two copies in each cell, the quantitative results obtained in molecular studies are evaluated by dividing it into two.[9,14-17]
Five healthy children (3 males, 2 females, 36.6±33.5 month) between six month and three years of age were selected for preparation of the standart curve in real-time PCR. They were recruited during routine pediatric outpatient visits for conditions not related to immunological or infectious diseases. All healthy control patients underwent a thorough clinical evaluation and were screened for a normal blood cell count.
The DNA was extracted from peripheral blood using the QIAamp DNA Blood Mini Kit (Qiagen GmbH, Hilden, Germany). The fragment of SJ KRECs was prepared by amplifying the DNA extracted from the blood of each child with specific primers (forward: 5'-TCC CTT AGT GGC ATT ATT TGT ATC ACT-3' and reverse: 5'-AGG AGC CAG CTC TTA CCC TAG AGT-3') and the specific primers for TR alpha constant TCRAC ( forward: 5 '-TGG C CT AAC CCT GAT CCT CTT-3' and reverse: 5'-GGA TTT AGA GTC TCT CAG CTG GTA CAC-3') using conventional PCR. After optimization studies, we determined an initial heating at 95°C for 2 min for KRECs, followed by 45 cycles of denaturation at 95°C for 10 sec, primer annealing at 58°C for 30 sec, and elongation at 72°C for 1 min. Additionally, final elongation step was performed at 72°C for 10 min by 1 cycle. Also, we used the same protocol for optimal PCR condition in TCRAC gene, except for primer annealing temperature being optimized at 62°C for 30 sec. We evaluated whether the correct genes after conventional PCR were obtained by gel electrophoresis for both genes (KRECs 90 b p, TCRAC 80 bp). The Qiaquick Gel Extraction Kit (Qiagen GmbH, Hilden, Germany) was used to purify amplification after gel electrophoresis.
Real-time PCR for KRECs and TCRAC
The absolute numbers of patient KRECs and
TCRAC at different periods were detected by a
real-time PCR assay performed on the real-time
PCR (Applied Biosystem Step One Plus) in
duplications. The SJ KREC forward primer (5'-TCC
CTT AGT GGC ATT ATT TGT ATC ACT-3') and
reverse primer (5'-AGG AGC CAG CTC TTA CCC
TAG AGT-3') and probe (5'-VIC-TCT GCA CGG
GCA GCA GGT TGG-TAMRA-3'), and TCRAC
(forward 5'-TGG CCT AAC CCT GAT CCT CTT-3',
reverse 5'-GGA TTT AGA GTC TCT CAG CTG
GTA CAC-3' and probe 5'-FAM-TCC CAC AGA
TAT CCA GAA CCC TGA CCC-TAMRA-3') were
designed. Primer specificities were checked by
Basic Local Alignment Search Tool (BLAST)
search (http://www.ncbi.nlm.nih.gov/blast/), which
confirmed their uniqueness.
We used a previous protocol designed by Sottini et al.[9] Briefly, PCR reactions were developed in a final volume of a 20 µL mixture, consisting of 10 ?L of 2× T aqMan U niversal P CR m aster m ix (AppliedBiosystems) and primers and probes for SJ KRECs at the f inal concentration of 900 n Mand 200 nM, respectively. Amplification of the TCRAC reference gene and KREC gene was performed in the same plate with the same concentrations of specific primers and probes. The KREC and TCRAC copy numbers were obtained by extrapolating the respective sample quantities from the standard curve obtained by serial dilutions (107, 105, 103, and 101) which were amplified in each PCR plate. A standard curve was included in every PCR reaction. The number of KRECs per 1 06 PBMC was calculated using the following formula:
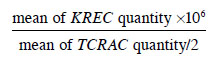
The mean quantity of TCRAC was divided by two, as there are two TCRAC g ene c opies i n e ach c ell; i.e., one for each chromosome. This value, together with the lymphocyte plus monocyte count (which were the cells obtained in PBMC preparation) in 1 mL of blood, was utilized to calculate the absolute number of KRECs per mL of blood (copies/mL) that i s = ( KRECs p er 1 ×106 PBMC) × (lymphocyte plus monocyte count in 1 mL of blood)/106. Each experimental procedure was accepted, only if the standard curve slopes ranged between -3.55 and -3.30, PCR efficiencies varied from 91 to 100%, and correlation coefficients (R2) were higher than 0.998.[9]
Treatment protocols
In immunosuppressive treatment after
transplantation, in addition to triplet therapy
comprising tacrolimus, mycophenolate mofetil, and
prednisolone, an induction therapy with basiliximab
20 mg was administered on the day of transplant
and four days post-transplant. After the end of the
transplantation, continuous infusion was started with
tacrolimus at a dose of 1 mg/kg/d and, then, continued
with oral administration of 0.025 mg/kg every 12 h.
Mycophenolate mofetil 1,000 mg was administered
in the operating room during the transplant.
Methylprednisolone 250 mg was administered prior
to implant and after the reperfusion and, then, for
the first postoperative days at a dose of 125 mg
intravenously three times, 1 mg/kg methylprednisolone
daily for one week and subsequently tapered to
prednisone 0.5 mg/kg/d. Thirty days after the LTx,
methylprednisolone was weaned by 5 mg every two
weeks and treatment was switched to prednisone
20 mg/day by six to eight weeks. The dose of
prednisone was reduced to 5 mg/day within three
months.
Statistical analysis
Statistical analysis was performed using the IBM
SPSS version 22.0 software (IBM Corp., Armonk,
NY, USA). Descriptive data were expressed in mean ±
standard deviation (SD), median (min-max) or number and frequency, where applicable. The Shapiro-Wilk
test was used to test the normal distribution assumption
of parameters. The Kruskal-Wallis test was used to
compare the non-normally distributed quantitative
attributes of diagnosed groups. The Mann-Whitney
U test was utilized to compare different groups"
non-normally distributed parameters such as sex, and
forced expiratory volume in 1 sec (FEV1) values of
the patients; intragroup comparisons of KREC, blood
parameters, age versus KRECs o vertime a nd s ex
versus KRECs overtime were performed using the
Wilcoxon signed-rank test. The Spearman correlation
analysis was used to investigate the dependence
between variables. A p value of <0.05 was considered
statistically significant.
Table 1. Patient characteristics
KRECs in patients before and after
transplantation
Real-time PCR results for KRECs were obtained
first by comparing with the standard curve from
KREC levels of DNA obtained from healthy
pediatric blood other than plasmid DNA. For both
genes, the calculation was made with the mean
values of the patients according to the number
of DNA copies in different dilutions. As a result,
the mean 24-h KRECs/106 P BMC w as h igher t han
before transplantation (5×105; 1×105) and on Day 7,
KRECs/106 PBMC was higher than the measurement at 24 h (45×105; 5×105), indicating that B cell kinetics
tended to increase after transplantation. However, the
difference was not statistically significant at different
time points (p>0.05) (Table 2).
Table 2. KREC production of patients before and after transplantation
KRECs in different disease groups
All patients were divided into groups according
to their primary indications, including idiopathic pulmonary fibrosis (IPF), chronic obstructive
pulmonary disease (COPD), and others. There was
no significant correlation between KREC numbers
among these groups (p>0.05) (Table 3 and Table 4).
Table 3. Statistical comparison of KRECs (106 PMBC) between the three primary indication groups
Table 4. Statistical comparison of KRECs (mL) between the three primary indication groups
KRECs according to age
Eleven patients were divided into two different age
groups and, on Day 7, KREC copies per 106 of blood were 836¥105 for the age group less than 45 years of
age, and 37¥105 for the age group over 45 years of age.
There was an only positive correlation between KRECs
copies per 106 of blood and age on Day 7 (p<0.05)
(Table 5).
Table 5. KRECs results according to age groups
KRECs according to sex
There were only three female patients. The analysis
of KREC results according to sex did not show
any significant differences in the number of KRECs
(p>0.05) (data not shown).
Correlation between KRECs and percentage of
FEV1
The FEV1 percentage is an important parameter
during the course of clinical follow-up of primary
disease and transplant follow-up for patients undergoing
LTx. We examined the relationship between the means
of KRECs and FEV1 percentage. Pre-transplantation
for patients were two separated groups according to
the percentage of FEV1 under 50 and over. There was
no significant correlation between KRECs and FEV1
percentage (p>0.05).
KRECs and blood count results of patients
When the lymphocyte absolute values of 11 patients
who underwent LTx were compared at 24 h and Day 7
and after the transplantation, the decline in the mean
lymphocyte count at 24 h was statistically significant
compared to the preoperative period (p=0.004). When
the absolute values of leukocytes are considered,
there was a statistically significant increase at 24 h
compared to pre-transplantation period (p=0.008).
On Day 7 after transplantation, the mean of absolute
leukocyte values decreased significantly compared to
ones at 24 h (p=0.026) (Table 6). There was a positive
correlation between the mean value of KRECs (mL)
and the mean value of lymphocytes at 24 h after
transplantation (p=0.043) (Table 7).
Table 6. Evaluation of lymphocyte and leukocyte levels in patients before and after transplantation
Four of the 11 patients died in the year following the transplantation with a one-year mortality rate of 36% and a survival rate of 64%. Unfortunately, we were not able to follow the patients for a longer period of time.
Monitoring early immune response in organ transplants is critical for acute rejections that occur after transplantation. This is an area of interest for both surgeons and immunologists. In 2015, a symposium was held on antibody-mediated rejection in cardiac transplants at the International Society for Heart and Lung Transplantation (ISHLT) meeting. Outcomes of this symposium is discussed in detail in an article published by Colvin et al.[18] As indicated, development of new markers for better diagnosis and follow-up of antibodymediated reactions are necessary in solid organ transplantations, and our preliminary study is a humble attempt in this respect.
Mansuroglu et al.[19] reported that cytoimmunological m onitoring o f p atients i s a non-invasive, easy and effective method in the early diagnosis of organ rejection after heart transplantation, particularly during hospitalization. The authors observed that changes in the CD4/CD8 ratio from the blood samples of the patients provided information about the infection or rejection.
In the present study, we examined the early immune response developed through B cells in patients undergoing LTx by current KREC assay procedure. The KREC is used as a marker for evaluating newly produced B lymphocytes. The KRECs consist of 50% of Ig light chain recombination of differentiated B cell progenitors and do not match their selves in subsequent B cell proliferation.[9] The KRECs can be assessed by molecular analysis for demonstrating the B cell outflow from bone marrow. With a very stable structure, the KRECs remain detectable in blood for a period of time and maintain it. The ratio between genomic coding part and signal part shows replication condition of subtypes of B lymphocytes and B cell neogenesis.[6,12] The quantification of KRECs was initially used to determine the number of developing B lymphocytes in the bone marrow of children with B-precursor or acute lymphoblastic leukemia treated with allogeneic human stem cell transplantation. However, as IGK gene deletion occurs physiologically in all B lymphocytes that fail to productively rearrange the IGK g enes o n one or both alleles, the number of KRECs h as b een proposed to be a quantitative marker of bone marrow output in all individuals.[8]
Piatosa et al.[10] described a pool of naïve CD19±IgD±CD27-B lymphocytes composing the largest B cell subset in all tested age groups (292 children and young adults aged 0 to 31 years, all of them healthy). While percentage of total B lymphocyte increases with age, it has been shown that naïve B lymphocyte subtypes were decreasing after age 2. Duchamp et al.[20] reported that the naive B-cells percentage declined between six months and eight years of age, and this definition of reference intervals for pediatric B-cell levels should facilitate the screening and diagnosis of various B-cell immunodeficiencies and the number of immature/ transitional and naïve B cells remains stable during adulthood.[21,22] Therefore, in the present study, we used pediatric blood samples to set-up our protocol and showed any change in KREC results to ensure that the level of naïve B lymphocytes was high and independent of the age-increasing antibody response.
The KREC levels are determinant i n developing immune response in pediatric patients with adenosine deaminase deficiency and in human immunodeficiency virus (HIV)-positive adult patients receiving retroviral treatment.[13,14] Detection of pre- and post-treatment quantity of KRECs is an indicator for reconstitution of the immune system.[14] In some of the European countries, the quantity of KRECs in pilot studies as a newborn screening test is used for characterizing diseases by identifying lymphopenia for newborns having immunodeficiency.[16,17] In a recent study, Kwok et al.[23] reported that the level of KRECs obtained by real-time PCR should be used in the diagnosis of primary immune diseases.
There are several studies detecting the level of KRECs after hematopoietic stem cell transplantation for primary immune deficiencies. These studies have shown that KRECs levels can be used for long-term follow-up of the B cell production.[12,15] It was found that most of the detectable B cells were transporting signal part, supporting the B cell neogenesis. Thus, duration of long-term intravenous Ig treatment after transplantation can be shortened and development of a personal protective treatment is possible. Due to prescribing intensive diets suppressing immune system and long-term Ig replacement treatment after LTx, KRECs analysis may serve as a very important tool for those patients.[15] In our study, KREC analysis was performed in blood samples in three different time-periods; before transplantation, 24 h after transplantation and on Day 7. When the results were compared between these time-periods, there was a quantitative difference in the mean values, although no statistically significant difference was found. An increase was detected in the KREC levels (per 106 cell) at 24 h and on Day 7 after transplantation compared to the KREC value before transplantation. There was no significant difference between the KREC levels before transplantation and at 24 h; however, an increase was found on Day 7. Considering that immunosuppressive treatments administered to patients undergoing transplantation have an impact on B cell production,[24] we believe that KREC analysis can be performed with longer follow-ups to demonstrate early adaptive immune response in transplantation patients.
The properties of immune system changes as one gets older, and some components of the immune system is less effective in elderly. It is well known that the response against infection and vaccine decreases in this population. It is demonstrated that different B type cells change by age and CD27+IgD+ cells that are IgM memory cells decrease in elderly.[25] A study by Serena et al.[26] consisting 37 adult patients with immunodeficiency and 78 healthy adults evaluated the KREC levels (copy count/106) with monocyte and lymphocyte values (mL) analyzed by real-time PCR method and indicated that, in the patient group, the median value of KRECs was lower than in the control group and no change was observed according to sex and age category. Similar to our study, no change was observed in relation to sex in the control group, while the KREC level was stable as the age increased. In our patient group, the KREC level (106) of the patients over the age of 45 years and average copy amount (mL) on Day 7 was higher than in patients under the age of 45 years. Along with aging, decrease in co-stimulatory molecules affecting B cells, defects in incoming signals to B cell receptors and reduction in helper T cell functions which are necessary for germinal center structure lead to reduction in the high affinity antibody response of B cells.[27] This can be explained with the decreased number of pre-B cells in bone marrow, despite the lack of any decrease in immature B cell division and transportation to periphery related to the age.
There is a need for a newly produced T and B lymphocyte resource for maintaining immunity in patients with chronic lymphocytic leukemia (CLL) which is characterized by B lymphocyte accumulation and result from Ig heavy chain mutations in organs such as bone marrow, lymph nodes, and spleen related to the defects of humoral and cellular immune response.[28] The KRECs cannot be found in cells having cellular division more than once without making a discrimination between normal and leukemic populations. The aforementioned study consisting of early-stage naïve-patients and control group found that lower quantity of KRECs per 106 PBMC compared to the control group was related to a decrease in newly produced B cells through dominance of enlarging leukemic cells.[28] It was also emphasized that the decreased number of KRECs in blood indicated a real decline in newly produced B cells in patients compared to controls. No significant correlation was found in the comparison of the increased rate of lymphocytes with KRECs levels in CLL patients. In the present study, despite the lymphocyte count at 24 h in the patient group, no significant decrease was found compared to pre-transplantation values. These results support the idea that changes in lymphocyte counts for patients undergoing LTx may also be related to KREC levels, indicating the interpersonal differences.[28]
Neutrophils play a very critical role in the pathogenesis of COPD and the increased neutrophil levels have been shown to be associated with pulmonary involvement. Even so, the relationship between the amount of peripheral blood cells of other leukocyte groups and pulmonary disease, allergy, and markers of airway obstruction is unclear. For this purpose, in a study evaluating the effects of leukocytes in peripheral blood on COPD symptoms and pulmonary functions, neutrophil counts were related to the increased symptoms related to chronic respiratory tract changes and decrease in FEV1 value.[29] In our study, the increase in neutrophil values between the timeperiods could be associated with pulmonary diseases, as well as increased chemokines due to degeneration of fibrous tissue of the lung. There was a correlation only at 24 h between blood parameters and KREC levels, KRECs/leukocyte number and KRECs/hemoglobin. It also showed the presence of active inflammation. A maximum increase in leukocyte cells and its relation to the increased KRECs copy counts at 24 hexplain the presence of inflammation. The FEV1 reflects the decrease in pulmonary functions and, thus, is an important marker in prognosis of pulmonary diseases. Acute rejection is typically characterized by decreased FEV1 value along with weakness, fever, cough, leukocyte increase, and gastrointestinal complaints. Tissue rejection may develop without any significant increase in the FEV1 value.[30] It is estimated that only 11% of the patients having a FEV1 value over 25%, which is accepted as the most important indicator for survival of patients undergoing transplantation, can survive more for a minimum of one year.[19] In the present study, a significant correlation could not be found between KREC levels of two groups having a FEV1 value under and over 50% before transplantation. Thus, we suggest that the patients should be followed at least until Day 7 of transplantation and further studies are necessary with the inclusion of FEV1 value after transplantation in long-term monitoring.
The main limitations to the present study include the limited number of patients due to lack of samples for all pre-determined time points, recent establishment of the LTx center, and limited research budget. Also, we were not able to follow patients for longer than a year.
In conclusion, the kappa-deleting recombination excision circle analysis is used for diagnosis of immunodeficiency disorders, particularly in demonstrating and observing immune system alterations after hematopoietic stem cell transplantation as an important tool for observation of B cell kinetics. Considering that survival rate is lower compared to other solid organ transplantations, long-term monitoring is of utmost importance in lung transplantation. In this preliminary study, the kappa-deleting recombination excision circle levels in relation to treatment modalities of the patients were not evaluated. Thus, measurement of kappa-deleting recombination excision circles within the B cell subtypes in future transplantations with more extensive patient groups would provide more insight into development of adaptive immune response following lung transplantation. The use of kappa-deleting recombination excision circles specific to different B cell subtypes as a routine biomarker may influence the prognosis and follow-up of the transplantation.
Acknowledgments: We thank Ass. Prof. Timucin Avsar (Bahçeşehir University, Istanbul, Türkiye) for his valuable contribution to real-time polymerase chain reaction optimization. The preliminary results of this study were presented as a poster in the 24th National Congress of Turkish Immunology Society which was held between April, 24 to 27th 2017 in Istanbul, Türkiye.
Ethics Committee Approval: The study protocol was approved by the Yeditepe University Hospital Ethics Committee (date: 10.09.2015, no: 37068608-6100-15-1113). The study was conducted in accordance with the principles of the Declaration of Helsinki.
Patient Consent for Publication: A written informed consent was obtained from each patient.
Data Sharing Statement: The data that support the findings of this study are available from the corresponding author upon reasonable request.
Author Contributions: Idea/concept: G.Y.D., C.A.K., A.Y., M.K.B, ZA.; Design: G.Y.D., C.A.K., A.Y., M.K.B.; Control/ supervision: G.Y.D., C.A.K., A.Y., M.K.B.; Data collection and/or processing: G.Y.D., Z.A.,M.K.B.,M.V., T.A.; Analysis and/or interpretation: G.Y.D., Z.A.; Literature review: G.Y.D., M.K.B., ZA.; Writing the article: Z.A., G.Y.D.; Critical review: G.Y.D., C.A.K., A.Y., M.K.B.; References and fundings: G.Y.D., M.K.B., ZA.; Materials: M.V., T.A., Z.A.
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding: The authors received financial support from the Scientific Committee of the Yeditepe University Hospitals in 2015.
1) Weill D, Benden C, Corris PA, Dark JH, Davis RD,
Keshavjee S, et al. A consensus document for the selection
of lung transplant candidates: 2014--an update from the
Pulmonary Transplantation Council of the International
Society for Heart and Lung Transplantation. J Heart Lung
Transplant 2015;34:1-15.
2) Dabak G, Şenbaklavacı Ö. History of lung transplantation.
Turk Thorac J 2016;17:71-5.
3) Trulock EP. Management of lung transplant rejection. Chest
1993;103:1566-76.
4) van Zelm MC, Szczepanski T, van der Burg M, van Dongen
JJ. Replication history of B lymphocytes reveals homeostatic
proliferation and extensive antigen-induced B cell expansion.
J Exp Med 2007;204:645-55.
5) Serana F, Chiarini M, Zanotti C, Sottini A, Bertoli D, Bosio
A, et al. Use of V(D)J recombination excision circles to
identify T- and B-cell defects and to monitor the treatment
in primary and acquired immunodeficiencies. J Transl Med
2013;11:119.
6) Bräuninger A, Goossens T, Rajewsky K, Küppers R.
Regulation of immunoglobulin light chain gene
rearrangements during early B cell development in the
human. Eur J Immunol 2001;31:3631-7.
7) González D, van der Burg M, García-Sanz R, Fenton JA,
Langerak AW, González M, et al. Immunoglobulin gene
rearrangements and the pathogenesis of multiple myeloma.
Blood 2007;110:3112-21.
8) Chiarini M, Zanotti C, Serana F, Sottini A, Bertoli D,
Caimi L, et al. T-cell receptor and K-deleting recombination
excision circles in newborn screening of T- and B-cell
defects: Review of the literature and future challenges. J
Public Health Res 2013;2:9-16.
9) Sottini A, Ghidini C, Zanotti C, Chiarini M, Caimi L,
Lanfranchi A, et al. Simultaneous quantification of recent
thymic T-cell and bone marrow B-cell emigrants in patients
with primary immunodeficiency undergone to stem cell
transplantation. Clin Immunol 2010;136:217-27.
10) Pi?tosa B, Wolska-Ku?nierz B, Pac M, Siewiera K,
Ga?kowska E, Bernatowska E. B cell subsets in healthy
children: Reference values for evaluation of B cell
maturation process in peripheral blood. Cytometry B Clin
Cytom 2010;78:372-81.
11) Mensen A, Ochs C, Stroux A, Wittenbecher F, Szyska
M, Imberti L, et al. Utilization of TREC and KREC
quantification for the monitoring of early T- and B-cell
neogenesis in adult patients after allogeneic hematopoietic
stem cell transplantation. J Transl Med 2013;11:188.
12) Lev A, Simon AJ, Bareket M, Bielorai B, Hutt D, Amariglio
N, et al. The kinetics of early T and B cell immune recovery
after bone marrow transplantation in RAG-2-deficient SCID
patients. PLoS One 2012;7:e30494.
13) Serana F, Sottini A, Chiarini M, Zanotti C, Ghidini C,
Lanfranchi A, et al. The different extent of B and T
cell immune reconstitution after hematopoietic stem cell
transplantation and enzyme replacement therapies in SCID
patients with adenosine deaminase deficiency. J Immunol
2010;185:7713-22.
14) Quiros-Roldan E, Serana F, Chiarini M, Zanotti C, Sottini
A, Gotti D, et al. Effects of combined antiretroviral
therapy on B- and T-cell release from production sites
in long-term treated HIV-1+ patients. J Transl Med
2012;10:94.
15) Li R, Xue C, Li C, Lou T, Tao Y, Li Y, et al. TRAC
variants associate with IgA nephropathy. J Am Soc Nephrol
2009;20:1359-67.
16) Shih HY, Krangel MS. Chromatin architecture, CCCTCbinding
factor, and V(D)J recombination: Managing longdistance
relationships at antigen receptor loci. J Immunol
2013;190:4915-21.
17) Kwan A, Church JA, Cowan MJ, Agarwal R, Kapoor N,
Kohn DB, et al. Newborn screening for severe combined
immunodeficiency and T-cell lymphopenia in California:
Results of the first 2 years. J Allergy Clin Immunol
2013;132:140-50.
18) Colvin MM, Cook JL, Chang P, Francis G, Hsu DT,
Kiernan MS, et al. Antibody-mediated rejection in cardiac
transplantation: Emerging knowledge in diagnosis and
management: A scientific statement from the American
Heart Association. Circulation 2015;131:1608-39.
19) Mansuroğlu S, Kırali K, Güler M, Tuncer A, Eren E,
Akıncı E, et al. Kalp transplantasyonlarında red fenomeninin
sitoimmünolojik monitörizasyon yöntemi ile izlenmesi.
GKDC Dergisi 1998;6:369-78.
20) Duchamp M, Sterlin D, Diabate A, Uring-Lambert B, Guérin-
El Khourouj V, Le Mauff B, et al. B-cell subpopulations in
children: National reference values. Immun Inflamm Dis
2014;2:131-40.
21) Olbrich P, de Felipe B, Delgado-Pecellin C, Rodero R,
Rojas P, Aguayo J, et al. A first pilot study on the neonatal
screening of primary immunodeficiencies in Spain: TRECS
and KRECS identify severe T- and B-cell lymphopenia. An
Pediatr (Barc) 2014;81:310-7.
22) Blanco E, Pérez-Andrés M, Arriba-Méndez S, Contreras-
Sanfeliciano T, Criado I, Pelak O, et al. Age-associated
distribution of normal B-cell and plasma cell subsets in
peripheral blood. J Allergy Clin Immunol 2018;141:2208-
19) e16.
23) Kwok JSY, Cheung SKF, Ho JCY, Tang IWH, Chu PWK,
Leung EYS, et al. Establishing simultaneous T Cell Receptor
Excision Circles (TREC) and K-Deleting Recombination
Excision Circles (KREC) quantification assays and laboratory
reference intervals in healthy individuals of different age
groups in Hong Kong. Front Immunol 2020;11:1411.
24) Bhorade SM, Stern E. Immunosuppression for lung
transplantation. Proc Am Thorac Soc 2009;6:47-53.
25) Martin V, Bryan Wu YC, Kipling D, Dunn-Walters D. Ageing
of the B-cell repertoire. Philos Trans R Soc Lond B Biol Sci
2015;370:20140237.
26) Serana F, Airò P, Chiarini M, Zanotti C, Scarsi M, Frassi
M, et al. Thymic and bone marrow output in patients
with common variable immunodeficiency. J Clin Immunol
2011;31:540-9.
27) Linton PJ, Dorshkind K. Age-related changes in lymphocyte
development and function. Nat Immunol 2004;5:133-9.
28) Motta M, Chiarini M, Ghidini C, Zanotti C, Lamorgese C,
Caimi L, et al. Quantification of newly produced B and T
lymphocytes in untreated chronic lymphocytic leukemia
patients. J Transl Med 2010;8:111.